Older Canadians have shouldered a disproportionately heavy burden of severe illness and death during the COVID-19 pandemic. As of September 16th, 2022, people over age 70 have accounted for 82% of all deaths, 35% of all intensive care admissions, and 50% of all hospital admissions due to SARS-CoV-2 infection in Canada (1).
Given these facts, we have synthesized CITF-funded and international research results to answer the following questions, which we hope you’re find interesting and valuable.
Residents in Canada’s long-term care (LTC) homes were particularly affected during the first two waves of the pandemic, which led to very high rates of severe illness and death.
How the first three waves unfolded in Canada’s LTC homes
| COVID-19 wave | LTC resident deaths | Impacts on LTC residents and interventions |
| The first wave March 1, 2020, to August 31, 2020
Dominant SARS-CoV-2 strain: wild-type (original) |
|
|
| The second wave
September 1, 2020, to February 28, 2021 Dominant SARS-CoV-2 strain: wild-type |
|
|
| The third wave
March 1, 2021, to August 15, 2021 Dominant SARS-CoV-2 strain: Alpha (higher transmissibility than wild-type) |
|
|
* Note that data from August 15, 2021, onwards for the other waves were not available at the time of writing. As of July 5, 2022, there were a total of 39,725 deaths in long-term care homes in Canada (12).
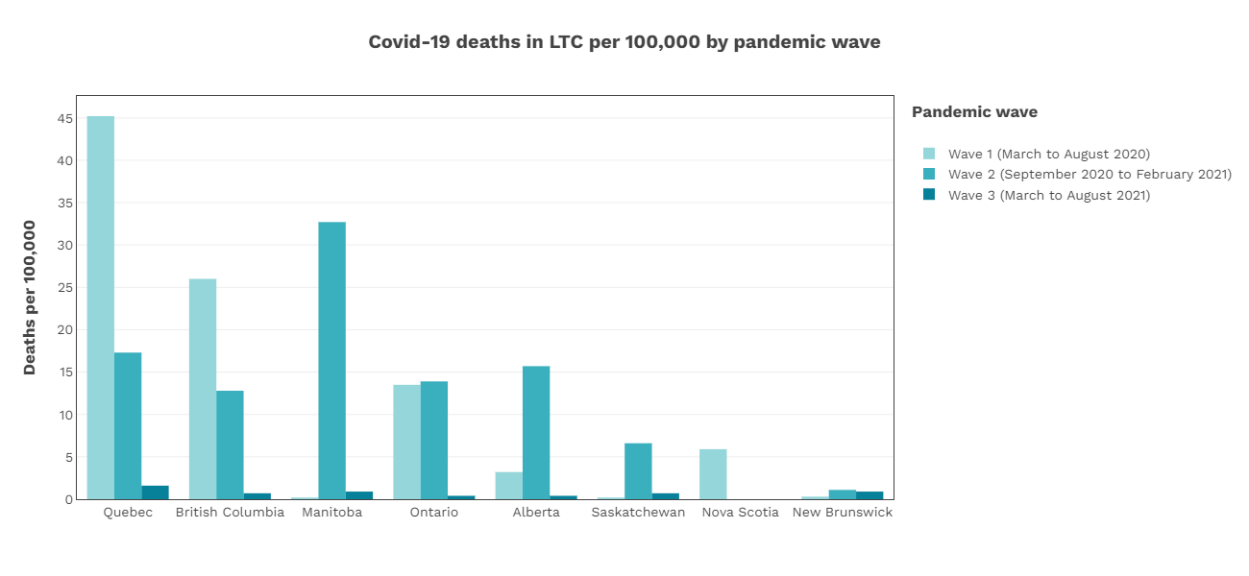
Figure 1 : COVID-19 deaths in long term care (LTC) homes per 100,000 people by pandemic waves.
(Adapted from Canadian Institute for Health InformationSources used by CIHI:
National Institute on Ageing. NIA Long Term Care COVID-19 Tracker , 2020–2021 (pandemic LTC deaths). Accessed August 17, 2021.
Alberta Health Services, accessed October 8, 2021, and Saskatchewan Ministry of Health, accessed September 14, 2021 (pandemic LTC deaths).
Statistics Canada. Population estimates, 2020. Accessed August 17, 2021.
, as accessed on 08/31/2022) (4).
Older people have experienced higher rates of severe disease and death due to COVID-19 throughout the pandemic
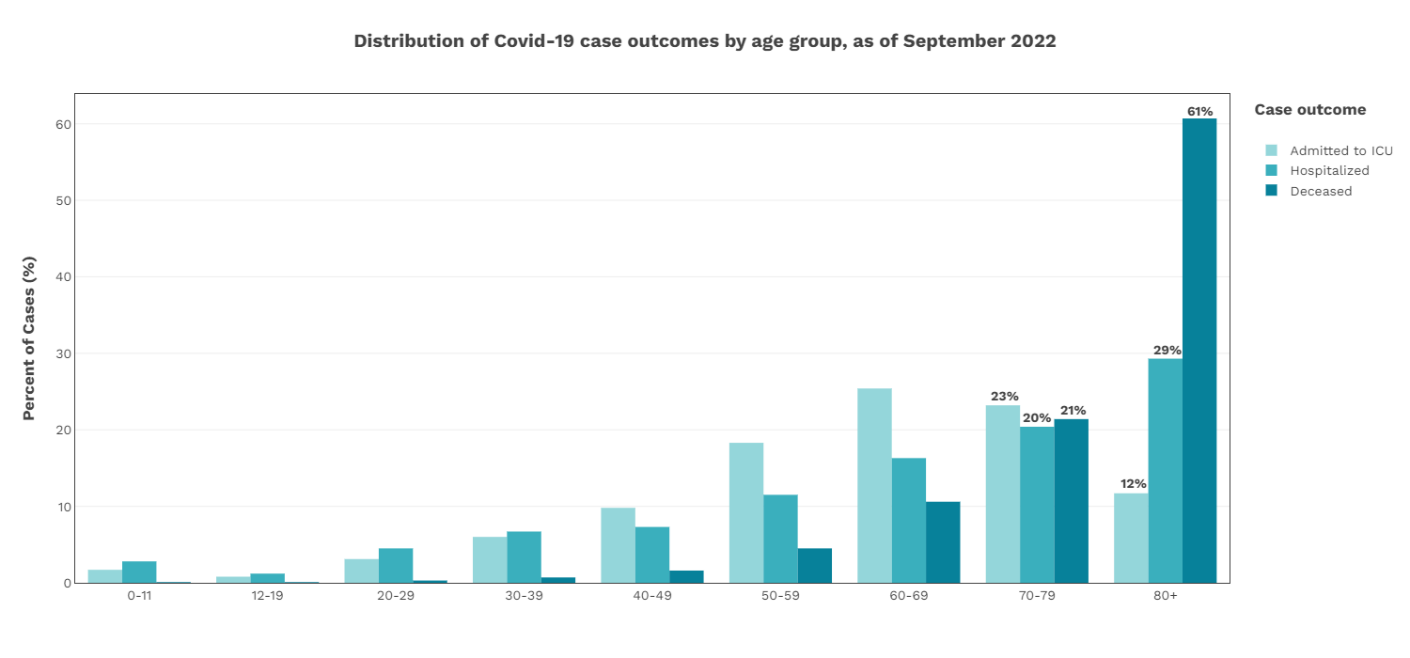
Figure 2 : Age distribution of COVID-19 deaths, hospitalizations, and ICU admissions in Canada as of September 16, 2022 (1) (adapted from Health Infobase Canada, as accessed on 09/21/2022).
By September 16th, 2022, the cumulative toll on older Canadians since the start of the COVID-19 pandemic had been very heavy:
- People over 70 years of age accounted for 82.1% of the total number of COVID-19 deaths reported in Canada, with those aged 80 years and older accounting for 60.7% (1).
- People over 70 years of age accounted for 49.7% of all hospitalizations associated with a SARS-CoV-2 infection in Canada, and 34.9% of intensive care admissions. Of these, people aged 80 years and older comprised 29.3% of all hospitalizations and 11.7% of all intensive care admissions (1).
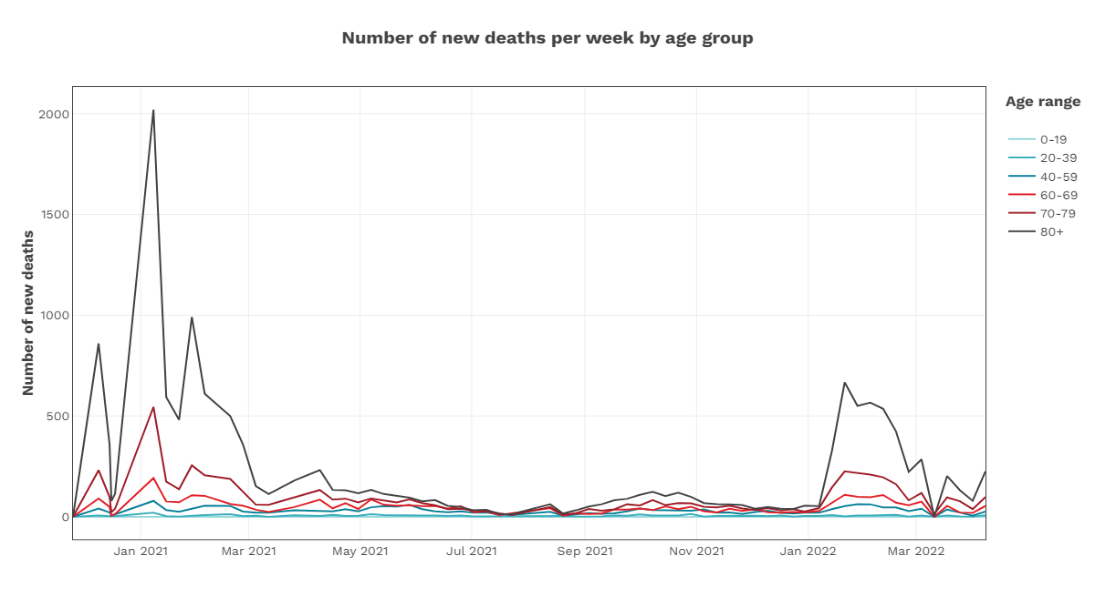
Figure 3 : COVID-19 weekly deaths from January 1, 2022 to September 1, 2022 in Canada across age groups (adapted from Health Infobase Canada, as accessed on 09/01/2022)
Older age, frailty, and comorbidities (other health issues) are the most common and significant risk factors leading to death from COVID-19.
- Frailty and older age correlated with higher rates of mortality in a group of COVID-19 patients with a median age of 71, according to a CITF-funded study from McNeil and colleagues (13).
- Older age is often accompanied by multiple underlying medical conditions that increase the risk of mortality from COVID-19 (14).
- Exact age and sex did not play a major role in determining who had an Omicron infection, as per a June 2022 preprint, not yet peer-reviewed, published by CITF-funded researchers Drs. Costa, Bowdish and colleagues. Their cohort had a median age of 87 years and were living in nursing and retirement homes (15).
- Particular characteristics of seniors’ residences (e.g., large capacity, the presence of long-term care units, and the provision of multiple services on-site) were independently associated with SARS-CoV-2 outbreaks, as shown by CITF-funded studies (16-18).
As of September 11th, 2022, more than 98% of Canadians aged 70+ had received two doses of COVID-19 vaccine. Of them, more than 88% had received an additional dose and 53% of those 70+ had received two additional doses of vaccine (19).
Two doses worked, but are no longer enough in older Canadians demic
- Three weeks after the first dose, older adults exhibited weaker antibody and neutralization responses compared to younger adults. However, two weeks after the second dose, their neutralization activity levels rebounded (20). These were findings by CITF-funded Wellness hub study researchers Drs. Allison McGeer, Sharon Straus, Anne-Claude Gingras, and team.
- Prior to the Omicron wave, two doses of vaccine were shown to be 52.5% effective against infection and 78.6% effective at preventing severe illness in LTC residents (21).
- The levels of neutralizing antibodies decline faster among older adults: a substantial decline, or waning, in antibody titers was observed among a cohort of older adults between three and six months post second dose (20) compared to a younger comparison group. The levels of neutralizing antibodies decline faster among older adults: a substantial decline, or waning, in antibody titers was observed among a cohort of older adults between three and six months post second dose (20) compared to a younger comparison group.
- Data compiled by the CITF showed that 10-35% of LTC residents did not develop detectable neutralizing antibodies after two doses of vaccine (20, 22).
- After two vaccine doses, older age was associated with lower levels of neutralizing antibodies compared to a matched group of younger individuals. In contrast, vaccination plus previous COVID-19 infection was associated with higher neutralizing antibody levels, according to findings from CITF-funded researchers Dr. Mark Brockman and colleagues (23).
Booster doses elicit major advantages to older Canadians
As immunity wanes over time, boosters came just in time for older Canadians. This addition to the original two-dose vaccine regimen has shown significant protection against severe disease and death from SARS-CoV-2 variants. Additionally, the booster doses protected LTC residents from the worst outcomes of the Delta and Omicron variants.
- Three COVID-19 vaccine doses reduced the risk of COVID-19 hospitalization by 90% among residents without a previous infection; a fourth dose of any mRNA vaccine decreased the risk of infection in LTC residents by 81%, according to research by CITF-funded research led by Drs. Costa and Bowdish (15).
- The antibody concentration in LTC residents increased significantly right after a third dose, but started to decline again, much like what was seen after the second dose, suggesting further doses were required, according to the CITF-supported team of Drs. Romney, Brumme and Brockman (24).
- One month after three vaccine doses, a weaker humoral response was observed in people with more chronic health conditions (24).
Moderna outperforms Pfizer in older Canadians, mixing-and-matching is OK and shorter dosing intervals are best for seniors
Both mRNA vaccines are very effective, though Moderna offers some advantages over Pfizer, according to international research, as well as research performed by several CITF-funded teams including Drs. Bowdish and Costa and a team led by Drs. McGeer, Straus, and Gingras:
- LTC residents who received Moderna’s Spikevax vaccine showed better antibody quality and a higher number of antibodies that lasted longer than LTC residents who received Pfizer’s Comirnaty vaccine (20, 22).
- LTC residents who received Moderna’s Spikevax made more CD4+ T cells, an indicator of immune memory, than those who received Pfizer’s Comirnaty vaccine (slide 51) (25).
- Two-dose regimens of the Moderna and Pfizer vaccines provided a high level of protection against COVID-19 hospitalizations in a real-world evaluation at 21 U.S. hospitals between March and August 2021. The research showed vaccine effectiveness (VE) against COVID-19 hospitalization was 93% with two doses of the Moderna vaccine and 88% with two doses of the Pfizer-BioNTech vaccine (26).
- In a result that suggests Pfizer may wane faster in older people, people 65+ who got the Pfizer vaccine between January to March 2021 had a higher death rate than those who got the Pfizer vaccine later (July 2021). Protection against death was sustained for the Moderna vaccine recipients (27).
- Three doses of Moderna was 47% more effective at protecting LTC residents against infection than three doses of Pfizer (15).
Four weeks after the second dose, mixing-and-matching mRNA vaccines (Pfizer and Moderna) and the AstraZeneca vector-based vaccine was not found to make a difference. Mixing-and-matching was not associated with significant differences in antibody responses, supporting their interchangeability, according to the CITF-funded UNCoVER study led by Dr. Donald Vinh (28).
Although longer dosing intervals have generally been found to be beneficial for younger people, there were upper limits to the benefit for older people with extended intervals. The immune impact of different dosing intervals was examined by CITF-funded studies of LTC residents:
- A longer dosing interval led to lower anti-RBD antibody levels over time, according to the StopCOV study in Ontario led by Dr. Sharon Walmsley (29).
- 16 weeks between the first and second dose was likely the upper limit for the dosing interval, especially in frail LTC residents who were not previously infected, according to the Montreal-based UNCoVER study (28).
Omicron is harder to neutralize than wild-type for all ages, even after three vaccine doses. However, the response against Omicron of older Canadians is comparable to that of younger Canadians after three doses, according to CITF-funded researchers (24, 30).
Omicron-specific neutralization, however, declined more rapidly in older adults following three doses when compared to younger adults. At six months post vaccination, neutralization was undetectable in 96% of COVID-19-naive older adults (31).
During the Omicron era, a fourth dose in older adults showed added effectiveness (95% of vaccine recipients received Moderna as the fourth dose). Seven days or more after a fourth dose, vaccine effectiveness was found to be 49% against infection, 61% against symptomatic infection and 86% against severe outcomes. This compares to the vaccine effectiveness 84 or more days after a third dose: 19% against infection, 31% against symptomatic infection, and 40% against severe outcomes. These data are from research by CITF-funded experts Drs. Andrew Costa and Jeffrey Kwong (32).
With the very high rates of immunity induced through vaccination in 2021, and over half of Canadians infected during the Omicron wave in 2022, hybrid immunity (immunity due to both infection AND vaccination) is the new norm. Studies so far have shown that the LTC residents who survive COVID, who don’t develop other co-morbidities due to the disease, and who have been vaccinated, have better immunity for a longer time than those who have only had an infection or only had vaccines.
- Those LTC residents with hybrid immunity (fully vaccinated AND had a SARS-CoV-2 infection in the fall of 2021 (within three months of the start of the Omicron wave) had more robust immunity: the risk of getting infected again decreased by 48%, according to a recent CITF-funded preprint (15).
- Previous infection with wild-type or the Delta variant was shown to induce high levels of neutralizing antibodies, which blocked reinfection by the same strain. However, antibodies from these blood samples had a reduced ability to neutralize Omicron (30).
- A breakthrough infection after vaccination has been found to confer better immune responses against reinfections by both wild-type and Omicron compared to three vaccine doses alone (31).
Previously, the only COVID-19 vaccines available in Canada were monovalent – tailored solely to the original novel coronavirus. The new bivalent shots from Moderna (called Spikevax Bivalent, tailored to Omicron B.1.1.529 (BA.1)) have now been approved by the Government of Canada for use in all adults age 18+ years (33). Health Canada is currently reviewing another bivalent booster candidate from Pfizer-BioNTech. for use in all adults age 18+ years (33). Health Canada is currently reviewing another bivalent booster candidate from Pfizer-BioNTech.
- Moderna’s first bivalent booster vaccine candidate demonstrated superior neutralizing titers compared to mRNA-1273 (Moderna’s monovalent vaccine) against all variants of concern, including Omicron BA.1 and BA.5. Superiority was maintained for six months after the booster (34).
- Those most likely to get severe disease – older people, the immunocompromised, and those with comorbid conditions like diabetes, kidney disease, and underlying lung disease – would benefit the most from bivalent booster doses.
A critical factor that may complicate efforts to contain COVID-19 through vaccination is “pandemic fatigue”. This phenomenon, characterized by demotivation to follow recommended protective non-pharmaceutical interventions (NPIs) such as mask wearing and social distancing, has been implicated as a factor in the recent spread of the virus.
- Modelling data have suggested that infections, hospitalizations, and deaths were highest when no one had been vaccinated (the baseline scenario) and lowest in cases where LTC homes had had residents vaccinated AND had strongly adhered to NPIs (35).Modelling data have suggested that infections, hospitalizations, and deaths were highest when no one had been vaccinated (the baseline scenario) and lowest in cases where LTC homes had had residents vaccinated AND had strongly adhered to NPIs (35).
- Ecological studies have suggested that the implementation of community-based masking policies at national and regional levels are associated with fewer COVID-19 infections, hospitalization, and mortality (36, 37). In a review article (38) it was observed that wearing a mask was associated with a significantly reduced risk of COVID-19 infection (OR= 38). Additionally, in healthcare workers, masking was associated with a reduced risk of infection by nearly 70% (38).
- Evidence shows that physical distancing of at least one meter lowers the risk of COVID-19 transmission compared to distances of less than one meter (aOR- 0.18). However, distances of two meters could be even more effective, suggesting that protection against COVID-19 transmission is increased as the distance is increased (change in relative risk- 2.02) (39-41).
- Hand hygiene can reduce the risk of infection from touching surfaces contaminated with viruses and bacteria (42, 43). Similarly, cleaning and disinfecting high-touch surfaces may help to reduce the presence of SARS-CoV-2 on environmental surfaces (44). Hand hygiene can reduce the risk of infection from touching surfaces contaminated with viruses and bacteria (42, 43). Similarly, cleaning and disinfecting high-touch surfaces may help to reduce the presence of SARS-CoV-2 on environmental surfaces (44).
Research so far has shown that immunity in older adults lasts three to six months (20, 22). Therefore, one could speculate that a booster will be needed roughly every six months after an immunity conferring event (either the last booster or a SARS-CoV-2 infection, whichever is last) to ensure adequate protection.
At this time, NACI guidelines suggest that a fall 2022 booster dose with any authorized COVID-19 vaccine will be most important for older adults and other populations at increased risk of severe COVID-19 disease regardless of the number of booster doses previously received (45).
“After you’ve had three doses, it isn’t about how many vaccines you’ve had, but how recently you’ve been vaccinated,” stated Dr. Bowdish. “Two doses are not enough to protect from severe Omicron infection so get the third dose as soon as you can. Protection against having a symptomatic Omicron infection wanes by three to five months following a booster vaccination. Therefore, if you’re able to get vaccinated at the start of a wave, you’ll be at your most protected right when you are most likely to get infected.”
According to Drs. Costa, Bowdish and their team, the only risk of too many boosters could arise from immune exhaustion, which is a loss of immune cell responsiveness to antigens due to excessive exposure to the same antigens. However, this phenomenon has never been observed following repeated vaccinations. Indeed, booster doses (i.e., beyond the first two doses) appear to be highly effective at preventing severe COVID-19 in older adults as they extend the period of immune protection.
Few researchers espouse that LTC residents and older Canadians should wear masks at all times. However, the strength of people’s immunity varies greatly depending on several factors, as seen above. Dr. Bowdish also commented that some older adults and people on immunosuppressive medications are not protected by vaccination at all. This can be because their immune systems cannot mount a strong enough response or because those responses decrease very quickly. The Omicron variants that are circulating now are particularly good at infecting people who have weaker responses to vaccination.
Dr. Bowdish offers this advice, based on her research:
- Wear a well-fitted mask indoors or in crowded areas: it’s a great way of protecting yourself and protecting your community.
- Avoid unventilated spaces and socialize outdoors as much as possible.
- Don’t postpone medical treatment. If you have a chronic health issue, the better you have that managed, the better you will do with any serious infection.
- Encourage friends and family to mask, socialize outdoors and keep their vaccines up to date. Do not socialize with people who have symptoms.
- Let politicians and leaders know that this is an important issue for you. Encourage them to follow-up on initiatives to increase air ventilation standards, provide masks and increase testing.
- Public Health Agency of Canada. COVID-19 epidemiology update 2022 [Available from: https://health-infobase.canada.ca/covid-19/].
- National Institute on Ageing. A cautionary tale: Canada’s vaccine rollout among older adults. Toronto, ON: National Institute on Ageing, Ryerson University; 2021.
- Canadian Institute for Health Information. The impact of COVID-19 on long-term care in Canada: Focus on the first 6 months. Ottawa, ON; 2021.
- Canadian Institute for Health Information. COVID-19’s impact on long-term care [Story] [Available from: https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/long-term-care].
- Clark J. Impacts of the COVID-19 pandemic in nursing and residential care facilities in Canada. June 10, 2021.
- Canadian Institute for Health Information. COVID-19 Intervention Scan [Product release] [Available from: https://www.cihi.ca/en/covid-19-intervention-scan].
- Canadian Division Joint Task. OP LASER- JTFC Observations in long term care facilities in Ontario Ontario; 2020.
- Graham J, Hosseini Z. Impacts of COVID-19 on Canadian nursing homes and seniors’ homes in 2021. September 13, 2022.
- Ontario Ministry of Health Ministry of Long-Term Care. COVID-19 testing for long-term care home staff 2020 [Available from: https://www.health.gov.on.ca/en/pro/programs/ltc/memo_20200716.aspx].
- CTV News Toronto. Ontario deploys rapid COVID-19 tests to long-term care homes in rural areas. November 24, 2020.
- Public Health Agency of Canada. COVID-19 vaccination in Canada 2021 [Available from: https://health-infobase.canada.ca/covid-19/vaccination-coverage/].
- Sinha SK, Doherty, R, McCleave, R, Dunning, J NIA Long term care COVID-19 tracker: National Institute on Ageing, Ryerson University; 2022 [Available from: https://ltc-covid19-tracker.ca/].
- Andrew MK, Godin J, LeBlanc J, Boivin G, Valiquette L, McGeer A, et al. Older age and frailty are associated with higher mortality but lower ICU admission with COVID-19. Canadian Geriatrics Journal. 2022;25(2):183-96.
- Banerjee A, Pasea L, Harris S, Gonzalez-Izquierdo A, Torralbo A, Shallcross L, et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020;395(10238):1715-25.
- Breznik JA, Rahim A, Kajaks T, Hagerman M, Bilaver L, Colwill K, et al. Protection from Omicron infection in residents of nursing and retirement homes in Ontario, Canada. medRxiv. 2022.
- Costa AP, Manis DR, Jones A, Stall NM, Brown KA, Boscart V, et al. Risk factors for outbreaks of SARS-CoV-2 infection at retirement homes in Ontario, Canada: a population-level cohort study. Canadian Medical Association Journal. 2021;193(19):E672-E80.
- Stall NM, Jones A, Brown KA, Rochon PA, Costa AP. For-profit long-term care homes and the risk of COVID-19 outbreaks and resident deaths. Cmaj. 2020;192(33):E946-e55.
- Brown K, Jones A, Daneman N, Chan A, Schwartz K, Garber G, et al. Association between nursing home crowding and COVID-19 infection and mortality in Ontario, Canada. medRxiv; 2020.
- Public Health Agency of Canada. Canadian COVID-19 vaccination coverage report. Ottawa September 16, 2022.
- Abe KT, Hu Q, Mozafarihashjin M, Samson R, Manguiat K, Robinson A, et al. Neutralizing antibody responses to SARS-CoV-2 variants in vaccinated Ontario long-term care home residents and workers. medRxiv. 2021.
- Williams C, Al-Bargash D, Macalintal C, Stuart R, Seth A, Latham J, et al. Coronavirus disease 2019 (COVID-19) outbreak associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) P. 1 Lineage in a long-term care home after implementation of a vaccination program—Ontario, Canada, April–May 2021. Clinical Infectious Diseases. 2022;74(6):1085-8.
- Breznik JA, Zhang A, Huynh A, Miller MS, Nazy I, Bowdish DM, et al. Antibody responses 3-5 months post-vaccination with mRNA-1273 or BNT163b2 in nursing home residents. Journal of the American Medical Directors Association. 2021;22(12):2512-4.
- Brockman MA, Mwimanzi F, Lapointe HR, Sang Y, Agafitei O, Cheung PK, et al. Reduced magnitude and durability of humoral immune responses to COVID-19 mRNA vaccines among older adults. The Journal of Infectious Diseases. 2021;225(7):1129-40.
- Mwimanzi F, Lapointe HR, Cheung PK, Sang Y, Yaseen F, Umviligihozo G, et al. Older adults mount less durable humoral responses to two doses of COVID-19 mRNA vaccine, but strong initial responses to a third dose. The Journal of Infectious Diseases. 2022.
- Bowdish D, Costa A. Summary report #4 How long does immunity to COVID-19 last? Waning immunity, boosters, and dosing intervals. 2022 January 24, 2022.
- Self WH, Tenforde MW, Rhoads JP, Gaglani M, Ginde AA, Douin DJ, et al. Comparative effectiveness of Moderna, Pfizer-BioNTech, and Janssen (Johnson & Johnson) vaccines in preventing COVID-19 hospitalizations among adults without immunocompromising conditions – United States, March-August 2021. MMWR Morb Mortal Wkly Rep. 2021;70(38):1337-43.
- Paz-Bailey G, Sternberg M, Kugeler K, Hoots B, Amin AB, Johnson AG, et al. Covid-19 Rates by time since vaccination during delta variant predominance. NEJM Evidence. 2022;1(3):EVIDoa2100057.
- Vinh DC, Gouin J-P, Cruz-Santiago D, Canac-Marquis M, Bernier S, Bobeuf F, et al. Real-world serological responses to extended-interval and heterologous COVID-19 mRNA vaccination in frail, older people (UNCoVER): an interim report from a prospective observational cohort study. The Lancet Healthy Longevity. 2022;3(3):e166-e75.
- Walmsley S, Szadkowski L, Wouters B, Clarke R, Colwill K, Rochon P, et al. Safety and efficacy of preventative COVID vaccines: The StopCoV study. medRxiv. 2022.
- Banerjee A, Lew J, Kroeker A, Baid K, Aftanas P, Nirmalarajah K, et al. Immunogenicity of convalescent and vaccinated sera against clinical isolates of ancestral SARS-CoV-2, beta, delta, and omicron variants. Med. 2022.
- Mwimanzi FM, Lapointe HR, Cheung PK, Sang Y, Yaseen F, Kalikawe R, et al. Brief Report: Impact of age and SARS-CoV-2 breakthrough infection on humoral immune responses after three doses of COVID-19 mRNA vaccine. medRxiv. 2022.
- Grewal R, Kitchen SA, Nguyen L, Buchan SA, Wilson SE, Costa AP, et al. Effectiveness of a fourth dose of covid-19 mRNA vaccine against the omicron variant among long term care residents in Ontario, Canada: test negative design study. BMJ. 2022:e071502.
- Dyer O. US and Canada to roll out the first omicron specific boosters within days. BMJ. 2022:o2144.
- Chalkias S HC, Vrbicky K, Walsh SR, Essink B, Brosz A, McGhee N, Tomassini JE, Chen X, Chang Y, Sutherland A, Montefiori DC, Girard B, Edwards DK, Feng J, Zhou H, Baden LR, Miller JM, Das R. A bivalent omicron-containing booster vaccine against Covid-19. N Engl J Med. 2022.
- Love J, Keegan LT, Angulo FJ, McLaughlin JM, Shea KM, Swerdlow DL, et al. Continued need for non-pharmaceutical interventions after COVID-19 vaccination in long-term-care facilities. Scientific Reports. 2021;11(1).
- Ju JTJ, Boisvert LN, Zuo YY. Face masks against COVID-19: Standards, efficacy, testing and decontamination methods. Adv Colloid Interface Sci. 2021;292:102435.
- Ford N, Holmer HK, Chou R, Villeneuve PJ, Baller A, Van Kerkhove M, et al. Mask use in community settings in the context of COVID-19: A systematic review of ecological data. EClinicalMedicine. 2021;38:101024.
- Li Y, Liang M, Gao L, Ayaz Ahmed M, Uy JP, Cheng C, et al. Face masks to prevent transmission of COVID-19: A systematic review and meta-analysis. Am J Infect Control. 2021;49(7):900-6.
- Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973-87.
- Jones NR, Qureshi ZU, Temple RJ, Larwood JPJ, Greenhalgh T, Bourouiba L. Two metres or one: what is the evidence for physical distancing in covid-19? Bmj. 2020;370:m3223.
- Public Health Agency of Canada Emerging Sciences Group. Evidence brief on SARS-CoV-2 virus dispersion distance [updated June 24 2020. Available from: https://cancovid.ca/resources/phac-esg/].
- Leslie RA, Zhou SS, Macinga DR. Inactivation of SARS-CoV-2 by commercially available alcohol-based hand sanitizers. American Journal of Infection Control. 2021;49(3):401-2.
- Ijaz MK, Nims RW, de Szalay S, Rubino JR. Soap, water, and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): An ancient handwashing strategy for preventing dissemination of a novel virus. PeerJ. 2021;9:e12041.
- Chen T. Fomites and the COVID-19 pandemic: An evidence review on its role in viral transmission. Vancouver, BC: National Collaborating Centre for Environmental Health. 2021.
- Public Health Agency of Canada. Recommendations on the use of bivalent Omicron-containing mRNA COVID-19 vaccines. September 1, 2022.

